Naming the Pain:
My Journey with Trigeminal Neuralgia
I first felt the pain in May of 2023.
At the time, I assumed it was dental. It had to be dental. I had just had a tooth pulled the month before, and that experience alone had taken so much out of me—emotionally, physically, financially. The dental journey was rough. Painful. Exhausting. And when this new pain appeared, my first thought wasn’t fear, it was fatigue.
I remember thinking:
I am not ready for another fight.
BUT
The pain was excruciating.
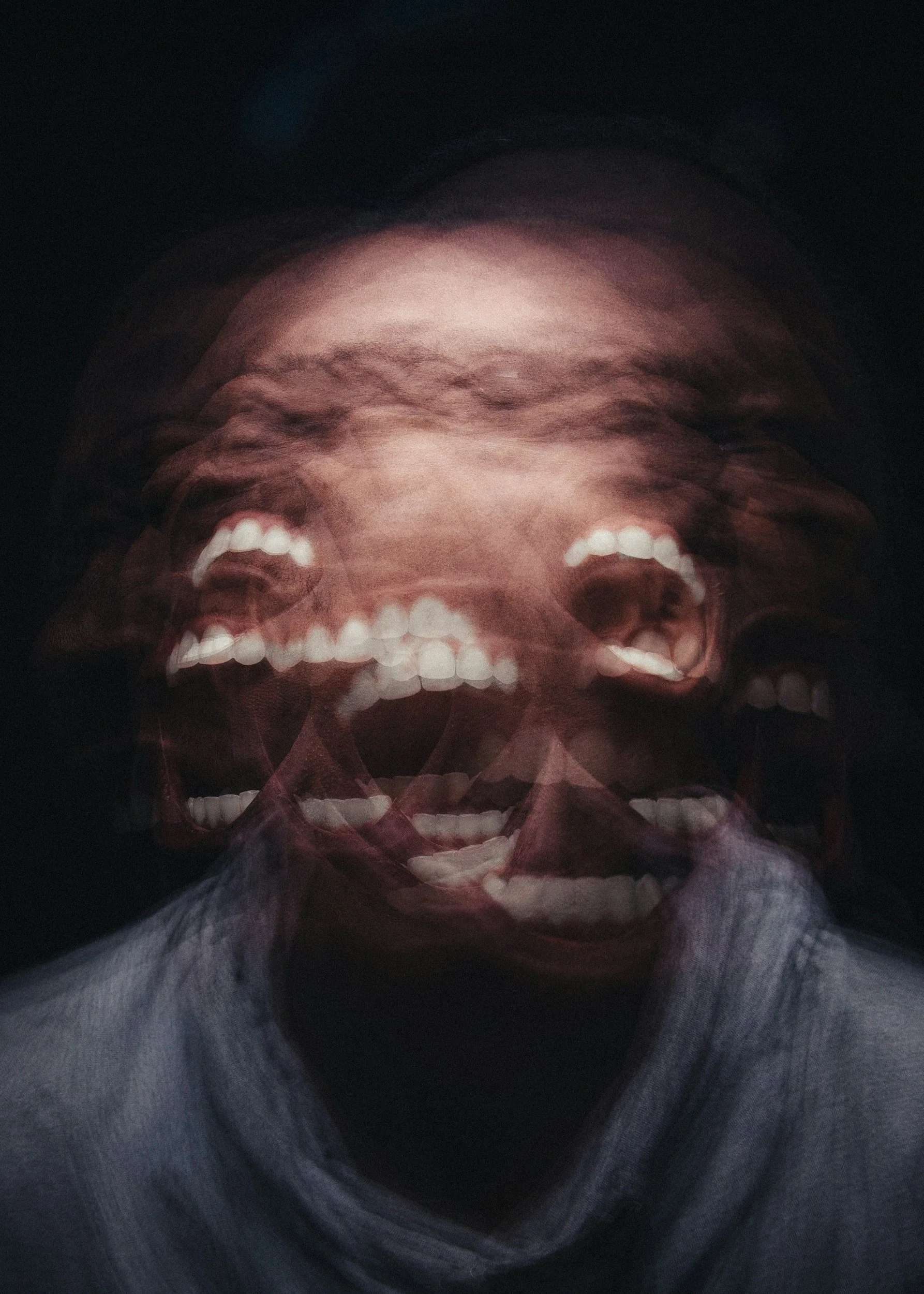
Trigeminal Neuralgia “The Suicide Disease”
There is a reason trigeminal neuralgia is often referred to as “the suicide disease.”
And it’s not because people with TN are weak.
It’s because unrelenting pain changes the human psyche.
Trigeminal neuralgia pain is not dull. It is not background discomfort. It is often described as electric shocks, stabbing, burning, or lightning bolts firing through the face—sometimes triggered by eating, brushing teeth, talking, wind, or even smiling. When pain is this severe, unpredictable, and intimate, it begins to erode a person’s sense of safety in their own body.
People don’t reach despair because they want to die.
They reach despair because they want the pain to stop.
Pain Without Insurance Is a Different Kind of Violence
In June of 2023, I lost my job.
And with it, I lost my health insurance.
What followed were long stretches—months—of excruciating, unmanaged pain. Pain that came and went. Pain that sometimes disappeared just long enough to give me false hope. Pain that returned without warning and dropped me to my knees.
I couldn’t pursue consistent care. I couldn’t chase specialists. I couldn’t afford answers. So I endured.
This lasted until November of 2024, when I finally got a new job with health insurance again.
By that point, I wasn’t just in pain—I was worn down by it.
Northwestern, Hope, and the First Dead End
Once I had coverage, I sought help at Northwestern Hospital, because they are known to have the strongest trigeminal neuralgia expertise in the Chicagoland area.
In December of 2024, I accidentally met with a surgical neurologist—the kind of specialist you typically only see after medication options fail. The correct order would have been to reach out to a regular neurologist but the current wait times for scheduling a new appointment is 6+ months. Scheduling with a surgical neurologist is much quicker. It only took me about a month to see this doctor, so the error was really a blessing in disguise.
She listened to my story, did a brief exam and ordered an MRI. The first step in getting a proper diagnosis. This was scheduled for January of 2025.
After that, the plan was simple:
Review the MRI results with a neurologist.
Figure out next steps.
Finally get relief.
But then—on the day of the appointment—it was canceled.
No real explanation.
No reschedule.
No urgency.
That cancellation cracked something in me.
I felt anger. Frustration. A familiar exhaustion. And for a while, I gave up again—not because the pain was gone, but because fighting systems while in pain is its own kind of injury.
Intermittent Pain Is Still Pain
For a while, the pain was intermittent.
I could go months without a flare-up.
That made it easier to minimize. Easier to push forward without care.
But in the fall of 2025, everything changed.
The pain began flaring up in a new area of my face, quadrant 3—along the jawline and teeth. It was intense. Deep. Relentless.
This time, I went to a dentist first, because I needed to be absolutely sure this wasn’t a tooth problem.
That dentist listened. Examined me. Took imaging. And then confirmed what I had already assumed:
This isn’t a dental issue. This is likely trigeminal neuralgia.
Seven More Months Wasn’t an Option
I tried again to make an appointment with a regular neurologist at Northwestern.
They told me the earliest available appointment was June of 2026.
That meant seven more months of pain.
Seven more months of flares.
Seven more months of endurance.
The logistics of healthcare in the United States is beyond cruel.
I was put on a waitlist.
And by luck—by grace—someone canceled.
I was able to be seen in November of 2025.
The Appointment That Changed Everything
My neurologist was excellent.
He listened patiently as I told my full story—starting in 2023, not just the most recent flare. He didn’t rush me. He didn’t minimize me. He offered insights, answered questions, and most importantly:
He wrote the prescription.
Oxcarbazepine.
This medication works by calming the overactive nerves responsible for trigeminal neuralgia pain. It doesn’t numb the face—it stabilizes the misfiring signals that cause those electric shock sensations.
The starting dose is typically 300mg.
The maximum dose is around 1800mg. The medication comes with side effects like most drugs:
Dizziness or lightheadedness
Fatigue / sleepiness
Headache
Nausea or vomiting
Double vision or blurry vision
Trouble with balance or coordination
Brain fog / slowed thinking
Tremor
Dry mouth
Doctors don’t like to prescribe doses higher than 1800mg because these symptoms worsen in a way that outweighs the benefits. Additionally, Low sodium (hyponatremia) is one of the most important risks with oxcarbazepine and can sneak up quietly. As a result, I have to get blood panels once a month to make sure my sodium levels are stable.
I started at 300mg.
It didn’t help.
I increased the dose to 600mg. Still nothing.
900mg and the relief began, but it didn’t last all day.
Within a month of initial dose adjustments I reached the recommended max of 1800mg.
And that’s when something unexpected happened.
Relief Came… and So Did Grief
At the maximum dose, the pain quieted.
And in that quiet, I realized something devastating:
I had been living with far more pain than I ever acknowledged.
The grief hit hard.
Grief for the years of endurance.
Grief for how strong I’ve had to be.
Grief for the way I’ve learned to normalize suffering because struggle has always been familiar.
There is something deeply frustrating about being so resilient that you don’t recognize when something has crossed the line into harm.
Being “strong” kept me going.
But it also kept me enduring what no one should have to endure.
COVID-19, Neurology, and a System at Capacity
There is increasing evidence linking COVID-19 to long-term neurological issues, including nerve inflammation and chronic pain conditions.
For more information:
CDC on long COVID neurological symptoms:
https://archive.cdc.gov/#/details?url=https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.htmlNIH research on COVID-19 and the nervous system:
https://www.ncbi.nlm.nih.gov/search/research-news/15736/
Neurology clinics are overwhelmed. Waitlists are long. And people like me are falling through the cracks—not because the doctors don’t care, but because the system is bottlenecked.
A Plea: We Need More Neurologists — and Fewer Barriers
We urgently need more neurologists.
But we also need to talk about why so few people enter or remain in this field:
The length and cost of training
Crushing student debt
High burnout from managing chronic, complex cases
Lack of diversity, which impacts whose pain is believed
The Core Policy Issue: The Medicare Residency Cap
In 1997, Congress passed the Balanced Budget Act, which froze the number of residency positions Medicare would fund at 1996 levels.
Why this matters:
Medicare funds the majority of U.S. residency training
Residency is the only pathway to becoming a neurologist
If you cap residencies, you cap future doctors — permanently
So even as:
the population grew
people lived longer
neurological disease increased
…the pipeline for neurologists did not expand.
This is one of the most consequential (and least publicly discussed) healthcare decisions in U.S. history.
Six months to a year for a neurology appointment is now normal in many U.S. cities — which is frankly dangerous.
My neurologist told me there is 1 neurologist for every 10,000 patients in the US. I double checked those stats and the ratio is currently closer to 1:20,000.
We cannot keep pretending this shortage is accidental.
It’s structural.
And patients are paying the price.
Learning to Listen Before It’s Too Much
Living with trigeminal neuralgia has taught me how to listen—really listen—to my body.
Not just to pain, but to the cost of endurance.
Not just to symptoms, but to the systems that delay care.
Not just to survival, but to what it takes to heal.
Relief is not a luxury.
Pain does not need permission to be real.
And strength should never require self-erasure.
If you are in pain and reading this: believe yourself sooner than I did.
